Diabetic retinopathy affects 80% of people who have been diabetic for 20 years or more. The disease accounts for 12% of all new cases of blindness each year in the West and is the leading cause for blindness in persons aged 20 to 64 years. Here are the symptoms, causes and treatments for diabetic retinopathy and how you can avoid going blind.
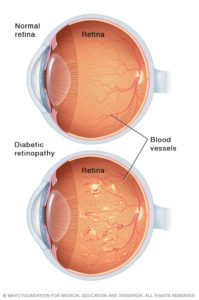 Diabetic retinopathy is damage to the blood vessels of the light-sensitive tissue at the back of your eye (retina). Your eyesight starts to fade and, if left untreated, you can end up blind.
Diabetic retinopathy is damage to the blood vessels of the light-sensitive tissue at the back of your eye (retina). Your eyesight starts to fade and, if left untreated, you can end up blind.
This medical condition can develop in anyone who has diabetes, whether type 1 or type 2. The longer you have the disease and the less controlled your blood glucose, the more likely you are to develop retinopathy.
The symptoms of diabetic retinopathy
When retinopathy starts developing you are unlikely to experience any symptoms or mild symptoms at the most.
Nevertheless, if you are diabetic and your vision changes suddenly, if it becomes blurry, spotty or hazy, you should consult your doctor right away.
The symptoms of diabetic retinopathy may include:
- blurred vision, making it hard to read or drive
- fluctuating vision, vision that gets worse and then better throughout the day
- floaters, dark spots or strings that float across your vision
- empty or dark areas in your vision
- poor colour vision
- gradually deteriorating vision
Diabetic retinopathy usually affects both eyes.
When you are first diagnosed as diabetic, you doctor should arrange for your eyes to be examined by a specialist to see whether you have retinopathy. Thereafter you should have your eyes tested once a year … for the rest of your life.
What causes diabetic retinopathy?
As all diabetics probably know, excess glucose floating around in your blood stream damages your blood vessels.
Your retina is a light-sensitive layer of tissue inside your eyeball. The optics of the eye (cornea and lens) creates an image of the visual world on the retina in a way that is similar to how an image is captured on a film in an old-fashioned (non-digital) camera.
Light striking the retina initiates a cascade of chemical and electrical events that trigger nerve impulses. These are sent to the visual centres of the brain through the optic nerve.
Excess sugar in your blood will, over time, damage the small blood vessels and nerve cells (neurons) of your retina. Thus careful management of your blood glucose levels is the best way of preventing diabetic retinopathy.
The damage caused by excess glucose leads to blockages in the tiny blood vessels of the retina. When the blood supply is cut off, the eye attempts to grow new blood vessels. But these blood vessels cannot develop properly and can easily leak.
There are two types of diabetic retinopathy:
- early diabetic retinopathy or non-proliferative diabetic retinopathy (NPDR)
- advanced diabetic retinopathy or proliferative diabetic retinopathy
Early diabetic retinopathy … non-proliferative diabetic retinopathy (NPDR)
In the early stages new blood vessels are not growing (proliferating).
Eventually, however, the walls of blood vessels in your retina will weaken and you will develop micro-aneurysms (tiny bulges) in the walls of the smaller vessels. These will leak fluid and blood into the retina.
Larger blood vessels will begin to dilate and develop irregular shape. Nerve fibres in the retina may also begin to swell.
NPDR can progress from mild to severe as more and more blood vessels become blocked. However, it does not normally require treatment unless macular oedema develops.
Macular oedema is the build-up of fluid in the macula, an area in the centre of the retina that is responsible for sharp, straight-ahead vision. Fluid build-up causes the macula to swell and thicken. This distorts your vision which can, if not treated promptly, be lost entirely.
Macular oedema is often treated with a laser to reduce the swelling. This is usually effective at stopping the development of the condition and sometimes it can reverse the loss of vision.
Advanced diabetic retinopathy … proliferative diabetic retinopathy
In the more advanced stages of retinopathy, damaged blood vessels close off. This causes the growth of new, abnormal blood vessels in the retina.
The damaged blood vessels can also leak into the vitreous, a gel-like substance that fills the centre of the eye and helps it maintain its round shape.
The growth of the new blood vessels will eventually stimulate the production of scar tissue. Scar tissue can cause the retina to detach from the back of the eye.
If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure an build up in the eyeball. This can damage the optic nerve that carries images from your eye to your brain and the result is glaucoma.
Glaucoma is a medical condition in which damage to the optic nerve leads to loss of vision and perhaps blindness. Indeed glaucoma is the leading cause of irreversible blindness in the world.
Glaucoma, however, develops slowly. Untreated glaucoma takes an average of 15 years to develop from initial damage to complete blindness so, with early detection and treatment, you can often protect yourself from serious loss of vision.
The goal of any treatment is to prevent loss of vision, as vision loss from glaucoma is irreversible. The condition can be treated with eye drops, pills, laser surgery, and traditional surgery.
How diabetic retinopathy is diagnosed
There are several ways your eyes can be checked for retinopathy:
A dilated eye exam … is the most common. In this examination, drops will be placed in your eyes to dilate (widen) your pupils so the examining ophthalmologist, a specialist eye doctor, can see the back of your eyes.
The drops will cause your vision to blur but will wear off after several hours. You should not drive or undertake other tasks that require good vision for 10 to 12 hours after the drops are put in.
During the examination, the ophthalmologist will look for signs of retinopathy … such as abnormal blood vessels in your retina, blood or fatty deposits in the retina, retinal swelling, bleeding into the vitreous, the growth of new blood cells or scar tissue, retinal detachment, and abnormalities in the optic nerve.
In addition, the ophthalmologist will measure you eye pressure to test for glaucoma and look for signs of cataracts. He may also give you an eye test.
In many parts of the world this kind of eye exam is undertaken by a mobile medical unit. A doctor will not be present. Instead the eye drops will be administered by a medical technician who will take photographs of your dilated pupils.
Later the photographs will be examined by a consultant ophthalmologist who will send you or your doctor a report on the condition of your eyes.
Fluorescein angiography … is a technique in which your eyes are dilated and photos are taken of the insides of your eyes. A doctor will then inject a special dye into your arm and take more photos as the dye circulates through your eyes. The images are used to find blood vessels that are broken, leaking fluid or blocked.
Optical coherence tomography … is another imaging test. OCT provides cross-sectional images of the retina that show its thickness. This helps determine whether fluid has leaked into the retinal tissue. An OCT examination can also be used to monitor the effectiveness of any treatment.
Treatment of diabetic retinopathy
There is no cure as such for retinopathy that arises from diabetes. The purpose of any treatment is to slow down or stop the progression of the condition.
The form your treatment will take will depend on what type of retinopathy you have and how severe it is.
If you have early diabetic retinopathy, you probably won’t need immediate treatment. However, your doctor will monitor your eyes with a dilated eye exam at least once a year.
Good blood glucose control can usually slow the progression of diabetic retinopathy when it is in the mild or moderate stages.
If you have advanced diabetic retinopathy or macular oedema, you will need surgery as soon as it is discovered. The kind of surgery will depend on the specific problems found in your retina.
Focal laser treatment (aka photocoagulation) … is a surgical technique that burns leaks from abnormal blood vessels using a laser. It can slow or stop the leaking of blood or fluid in your eye. It is usually performed in an eye clinic in a single session.
If your vision was blurred due to macular oedema, this procedure might not return your vision to normal but it is likely to prevent the oedema from getting worse.
Scatter laser treatment (aka pan-retinal photocoagulation) … can shrink abnormal blood vessels. In this surgical technique, areas of the retina that are away from the macula are subjected to laser burns. This causes the abnormal new blood vessels to shrink and scar. It is usually performed in an eye clinic in two or more sessions.
Your vision will be a bit blurry for a day or so after the procedure. You may also experience some loss of night vision or peripheral vision but the surgery should prevent your retinopathy from getting much worse.
Vitrectomy … is a surgical procedure in which a tiny incision is made in your eye to enable blood in the middle of the eye or scar tissue that is tugging on the retina to be removed. It is done in a hospital under local or general anaesthesia (depending on how tough you are feeling).
Surgery can slow or stop the progression of retinopathy. But it is not a cure. Diabetes is a lifelong condition, so retinal damage and loss of vision are still possible in the future. The trick is to get your blood sugar under full control.
Risk factors for diabetic retinopathy
Anyone who has diabetes is at risk of developing retinopathy. In fact, the longer you have diabetes (whether type 1 or type 2), the greater your risk of developing the disease.
Here are some other factors that increase your risk:
- you are of African descent, Native American or Hispanic
- you fail to control your blood glucose levels properly
- you fail to control your blood pressure
- you have high cholesterol
- you smoke tobacco
You cannot control your lineage nor how long you have had diabetes … but you are well positioned to control the other four factors above.
Your risk of developing diabetic retinopathy also increases when you are pregnant.
How to prevent diabetic retinopathy
You cannot really prevent diabetic retinopathy from developing. But you can prevent severe loss of vision from occurring. Here are some common-sense actions you can take:
Take control of your diabetes … follow the Beating Diabetes diet (low fat, low sugar, low salt, high GI, etc) and get at least 30 minutes of moderate aerobic activity (eg, walking) a day.
Monitor your blood glucose levels … by checking and recording your blood sugar levels at least 5 times a day, on arising and two hours after each meal. Your target range is 5 to 7 mmol/L (90 to 126 mg/dl). If your readings are outside these limits adjust your diet or exercise habits.
Monitor your HbA1c regularly … the results of a glycated haemoglobin test reflect how well you have been able to control you blood glucose levels over the previous two to three months. You should have it done at least three times a year (every four months). If you are taking good care of your blood glucose levels you should have a HbA1c level of less than 42 mmol/mol (6.0%).
Control your blood pressure and cholesterol levels … as a diabetic you have an 85% chance of having hypertension (excessive blood pressure) and too much cholesterol. Ongoing excessive blood pressure and high levels of LDL (‘bad’) cholesterol can cause just as much damage to your eyes as diabetes alone. Get them under control by losing weight, following the Beating Diabetes diet and exercising regularly.
Smoking … stop! Smoking dramatically increases your risk of diabetic retinopathy and other complications relating to diabetes.
Watch out for changes in the acuity of your vision … if you vision becomes blurred or hazy or spots appear, get medical advice immediately. The quicker you do so, the better the chances of avoiding severe damage to your eye-sight. Don’t put it on the long finger.